The European Society for Reproductive Medicine and Embryology (ESHRE) established good practice recommendations providing a definition for recurrent implantation failure (RIF) together with recommendations on how to investigate causes and how to improve the chances of a pregnancy.
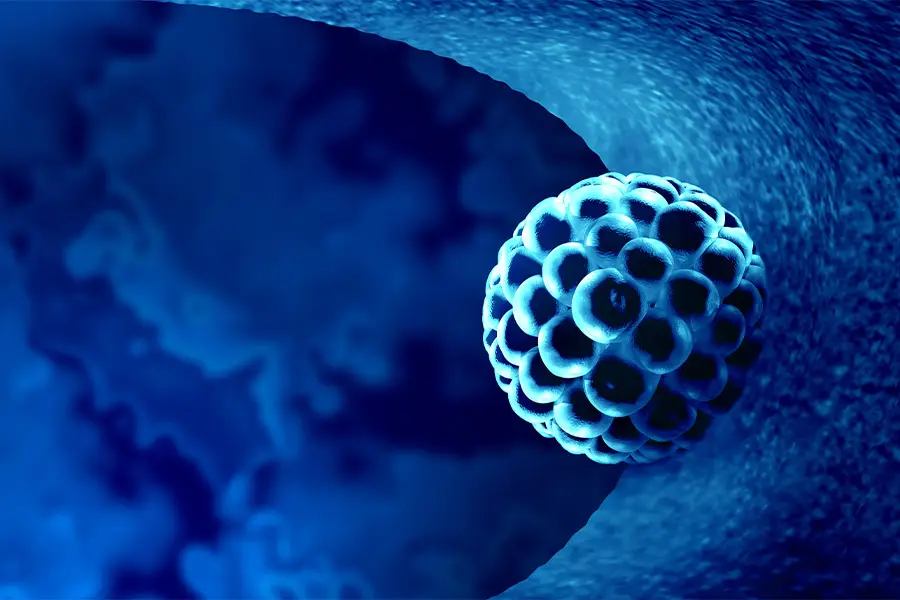
Definition of recurrent implantation failure
There is a lack of consistency in the clinical definition of RIF. The key factors that need to be considered while establishing the definition of RIF are the number of embryos transferred, whether the transferred embryos are genetically tested, and maternal age. In general, a patient considered to have RIF and needs to be investigated include:
- Transfer of euploid (genetically normal) embryos:
Transfer of 2 embryos regardless of the age of the woman. - Transfer of embryos of unknown euploidy:
Transfer of 3 embryos in women less than 35 years of age.
Transfer of 4 embryos in women between 35 to 39 years.
Transfer of 6 embryos in women more than 40 years.
Investigations for RIF
Multiple factors and causes for RIF have been suggested and studied. However, there is insufficient evidence to permit clear guidelines to be used for investigation and management of RIF. Investigations for RIF include investigating both female and male factors.
- Recommended
a. Review lifestyle factors (both partners).
b. Re-assessment of endometrial thickness is recommended. A review of the estradiol treatment regimen is recommended if the endometrium is noted to remain thin. Hysteroscopy to rule out Asherman’s syndrome can be considered.
c. Assessment of APA (antiphospholipid syndrome) and APS is recommended in RIF women with additional risk factors for thrombophilia, and can be considered in women without such risk factors. - Can be considered
a. Karyotyping (both partners) to confirm the absence of a chromosomal abnormality in parents. If a chromosomal abnormality is detected, genetic counselling and, where relevant, preimplantation genetic testing (PGT), is recommended.
b. 3D ultrasound.
c. Hysteroscopy when there is a suspicion of a uterine anomaly visualized on transvaginal ultrasound.
d. Endometrial function testing: While there are insufficient data to recommend the routine use of any commercially available test of endometrial receptivity to diagnose the cause of RIF, assessment of specific aspects of endometrial function by testing can be considered.
e. Assessment for chronic endometritis (CE) can be considered. If CE is diagnosed, treatment with antibiotics can be considered.
f. Assessment of thyroid function.
g. Assessment of late follicular and mid-luteal progesterone levels. - Not recommended
a. There are insufficient data to recommend the routine measurement of vitamin D levels or treatment of vitamin D deficiency
b. Uterine and vaginal microbiome profiling
c. Peripheral and uterine NK cell testing
d. Uterine T lymphocytes assessment
e. Blood cytokine levels assessment
f. HLA-C compatibility
g. Sperm DNA fragmentation
Interventions for RIF
- Recommended
a. Review estradiol treatment if endometrial lining remains thin
b. Patient care and counselling are recommended since women with RIF have been reported to have significantly higher levels of stress as compared to fertile healthy controls and admitted to feelings of social isolation and sensitivity to comments.
c. Optimizing lifestyle factors - Can be considered
a. Preimplantation genetic testing for aneuploidies (PGT-A)
b. Blastocyst-stage embryo transfer
c. Antibiotics if chronic endometritis is diagnosed - Not recommended
a. Intentional endometrial injury
b. Immunomodulation such as granulocyte colony stimulation factor (G-CSF) administration (either intrauterine or subcutaneous) , intravenous intralipid infusion, intravenous immunoglobulin (IVIG)
c. Intrauterine autologous peripheral blood mononuclear cells (PBMCs) infusion
d. Intrauterine platelet-rich plasma (PRP) infusion
e. Intrauterine hCG injection
f. Low molecular weight heparin (LMWH)
g. GnRH agonist and aromatase inhibitor pre-treatment
h. Assisted hatching
Reference: Human Reproduction Open, 2023, 2023(3), hoad023