Egg Freezing
Empowering you to take control of your fertility
Egg freezing with NOW-fertility
Free AMH test with egg freezing consultation
For a limited period, if you are based in either the UK or UAE, we are offering you a free of charge AMH test when you book an egg freezing consultation with one of our fertility experts.
NOW-fertility - Providing optimal support for the best chance of success
- No waiting time to start treatment
- Access to the best clinics worldwide with high success rates and latest technologies
- Virtual consultations at times to suit you
- Multilingual and experienced team
- Personalised care for your individual needs and preferences
- Transparent and affordable pricing
How does it work with NOW-fertility?
- Your first step will be a consultation with your consultant to discuss the best options for you, and with your nurse to ensure that all your screening tests and consent forms are completed.
- You are then ready to start the hormone treatment to stimulate your ovaries. The response to treatment will be assessed by ultrasound scans which can be arranged close to your home or work.
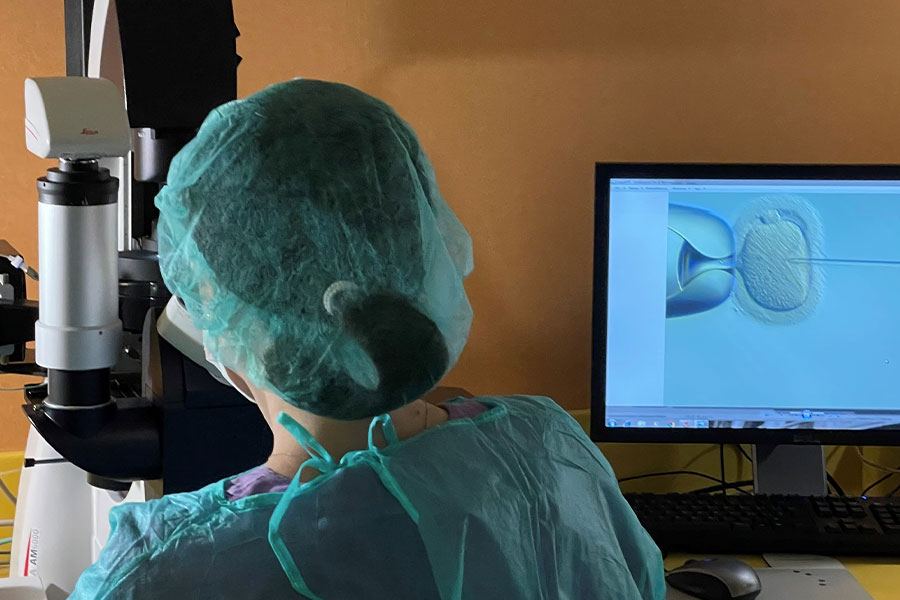
- You will travel to your chosen clinic for harvesting the eggs. These will be frozen and stored for possible future use.

Is egg freezing right for me?
- Social reasons to delay childbearing
- Medical reasons to preserve fertility before undergoing cancer treatment (chemo- and/or radio-therapy, or surgery)
- Ovarian cysts that may increase the risk of damaging the ovary
- Family history of premature ovarian failure
- Religious and/or ethical considerations that don’t allow embryo freezing
- Donating eggs to a known or unknown recipient
Where can I freeze my eggs with NOW-fertility?
- Egypt
- Greece
- Italy
- Poland
- Saudi Arabia
- Spain
- Tunisia
- UAE
- UK
Contact NOW-fertility to learn more about Egg Freezing
Our care team are here to explore your fertility journey and guide you through your options.
Our expertise in egg freezing
Our team at NOW-fertility consists of professional and multilingual care coordinators, nurses and consultants with extensive experience in fertility treatment and preservation.
We offer affordable egg freezing at a choice of the very best fertility clinics around the world with consistently high success rates, quality measures, experienced staff and state of the art facilities.
We can assist you to transfer your eggs between clinics in different countries if you wish to do so at any time in the future.







Why we are different
- Global network of clinics
- Treatment personalised to you
- Transparent, individualised pricing
- Virtual appointments & enhanced monitoring
- Multilingual expert team
Ready to start your journey?
Our commitment is to make fertility care accessible, successful and stress free for patients.
If you are ready to start your journey, book a consultation with one of our experienced fertility consultants.




